A complete guide to relieving rhinitis
Outline
– Understanding rhinitis: types, symptoms, and everyday impact
– What triggers rhinitis? Allergens, irritants, and the body’s response
– Getting a diagnosis: history, testing, and when to seek care
– Relief toolbox: home strategies and evidence-based treatments
– Living well with rhinitis: prevention, routines, and special situations
Introduction
Rhinitis is a common condition with uncommon ripple effects. Beyond the familiar runny nose and sneezing, it can drain energy, dim focus, and turn sleep into a stop-start affair. The good news is that most people can improve symptoms with a clear plan that matches their type of rhinitis, lifestyle, and environment. This guide walks you through the essentials: what rhinitis is, what sets it off, how professionals sort through causes, and which strategies tend to help in real life. Whether you’re dealing with seasonal flares or year-round congestion, you’ll find practical steps and balanced explanations designed to help you breathe more comfortably and live with fewer interruptions.
Understanding Rhinitis: Types, Symptoms, and Everyday Impact
Rhinitis refers to inflammation or irritation of the nasal lining, typically presenting with congestion, sneezing, runny nose, itching, and postnasal drip. While the symptoms overlap, the causes vary. Broadly, rhinitis can be grouped into allergic rhinitis, nonallergic rhinitis, mixed rhinitis, and infectious rhinitis. Allergic rhinitis is driven by an immune response to allergens such as pollens, dust mites, animal dander, or molds. Nonallergic rhinitis covers a range of triggers—from strong odors and air pollutants to weather changes and hormonal shifts—without the classic allergic antibody (IgE) pathway. Mixed rhinitis is exactly what it sounds like: a combination of allergic and nonallergic features. Infectious rhinitis usually follows a cold and often resolves as the viral illness runs its course.
Symptoms can be persistent or episodic. Some people notice a clear seasonal pattern tied to tree, grass, or weed pollens; others struggle all year, especially if dust mites or indoor molds are involved. Typical features include:
– Congestion that may shift sides
– Watery discharge, sometimes thickening during infections
– Sneezing bursts and nasal itch (more common in allergic rhinitis)
– Postnasal drip causing throat clearing or cough
– Reduced sense of smell during flares
Beyond discomfort, rhinitis has everyday consequences. It can disturb sleep, reduce concentration at work or school, and make exercise or outdoor time less enjoyable. In surveys, many adults report productivity dips on high-symptom days, and parents often notice that children with frequent congestion are more restless at night. Rhinitis also interacts with other conditions: it may worsen asthma control, contribute to sinus pressure, or amplify headaches. Notably, the severity of congestion doesn’t always match the irritation a person feels; even mild swelling can create a sense of “blocked” airflow because the nose is a finely tuned airflow regulator. Understanding which type of rhinitis you have and how it affects your day is the first step in shaping a practical, sustainable plan.
What Triggers Rhinitis? Allergens, Irritants, and the Body’s Response
Triggers fall into two broad camps: allergens that provoke an immune response and nonallergic irritants that stir up nasal nerves and blood vessels. Seasonal allergens include tree pollens in spring, grasses in late spring to summer, and weeds such as ragweed in late summer to fall (timing varies by region). Perennial allergens live with us year-round: dust mites thrive in bedding and upholstery, pet dander clings to carpets and clothing, and molds favor damp corners or poorly ventilated spaces. Outdoors, mold counts can spike after rain and in leaf piles. Even if you don’t have classic allergies, these exposures may still aggravate sensitive nasal tissue.
Nonallergic triggers are diverse:
– Airborne irritants: tobacco smoke, exhaust, cleaning products, perfumes, and industrial fumes
– Weather and environment: cold, dry air; sudden temperature shifts; low humidity in winter
– Physiologic changes: hormonal fluctuations in pregnancy or thyroid disorders
– Foods and beverages: spicy meals or hot soups can prompt “gustatory” rhinitis via reflex pathways
– Medications: a few drug classes may worsen congestion or rhinorrhea in susceptible people
– Mechanical factors: a deviated septum or turbinate enlargement can add to obstruction
In allergic rhinitis, the immune system produces IgE antibodies that recognize specific allergens. On exposure, mast cells in the nasal lining release histamine and other mediators, leading to itching, sneezing, swelling, and mucus production. A later phase—a few hours after exposure—can prolong congestion through continued inflammation. Nonallergic rhinitis often involves heightened sensitivity of nasal nerves and blood vessels. Triggers such as cold air or strong odors create a neural reflex that dilates vessels and boosts glandular secretion, even without an immune-allergen handshake. This helps explain why two people in the same room can react very differently to the same fragrance or temperature change.
Humidity, particle size, and airflow also matter. Dry air thickens mucus and slows ciliary movement, the tiny hairlike motions that clear the nose. Smaller particles stay airborne longer and travel deeper into nasal passages. Meanwhile, rapid shifts from warm to cold air can transiently swell nasal tissues. Understanding these mechanics gives you leverage: by managing indoor humidity, ventilation, and dust reservoirs, you can lower exposure intensity and reduce symptom cascades.
Getting a Diagnosis: History, Testing, and When to Seek Care
A thoughtful history untangles the rhinitis puzzle. Start by charting when symptoms occur, how long they last, and what seems to provoke or ease them. Note seasonal patterns, indoor versus outdoor differences, and responses to activities like cleaning, exercising, or traveling. It helps to record:
– Main symptoms (congestion, rhinorrhea, itching, sneezing, postnasal drip)
– Timing (morning peaks, nighttime worsening, weekend improvements)
– Environment (pets, carpets, bedding, workplace exposures, damp areas)
– Coexisting issues (asthma, headaches, snoring, reflux)
– Medication use and whether symptoms changed after starting new drugs
During an exam, a clinician looks for swollen turbinates, pale or bluish mucosa (often seen in allergic rhinitis), or redness typical of irritation. Clear, watery discharge leans toward allergic or nonallergic rhinitis, whereas thick yellow-green mucus may accompany viral infections; however, color alone doesn’t prove bacteria. Tenderness over sinuses or dental pain can hint at sinus involvement. When allergies are suspected, skin prick testing or blood tests for specific IgE can identify relevant allergens. These tests guide targeted avoidance steps and eligibility for allergen immunotherapy when appropriate. Nasal endoscopy is sometimes used to assess anatomy or rule out polyps, and imaging is reserved for complications or atypical features rather than routine cases.
Red flags that warrant timely evaluation include persistent unilateral blockage, frequent nosebleeds, facial swelling, high fever, severe pain, or symptoms that fail to improve despite basic measures. In children, mouth breathing, snoring, or school concentration issues may merit attention. Adults with asthma that worsens during allergy seasons often benefit from coordinated care because upper and lower airways influence each other. A clear diagnosis avoids trial-and-error spirals; it helps match treatments to the underlying mechanism—immune-driven, irritant-triggered, infectious, structural, or mixed—and sets realistic expectations for relief. If you are unsure whether your symptoms relate to allergies, a short, guided trial of certain therapies can be informative, but structured testing provides more confidence and reduces guesswork.
Relief Toolbox: Home Strategies and Evidence-Based Treatments
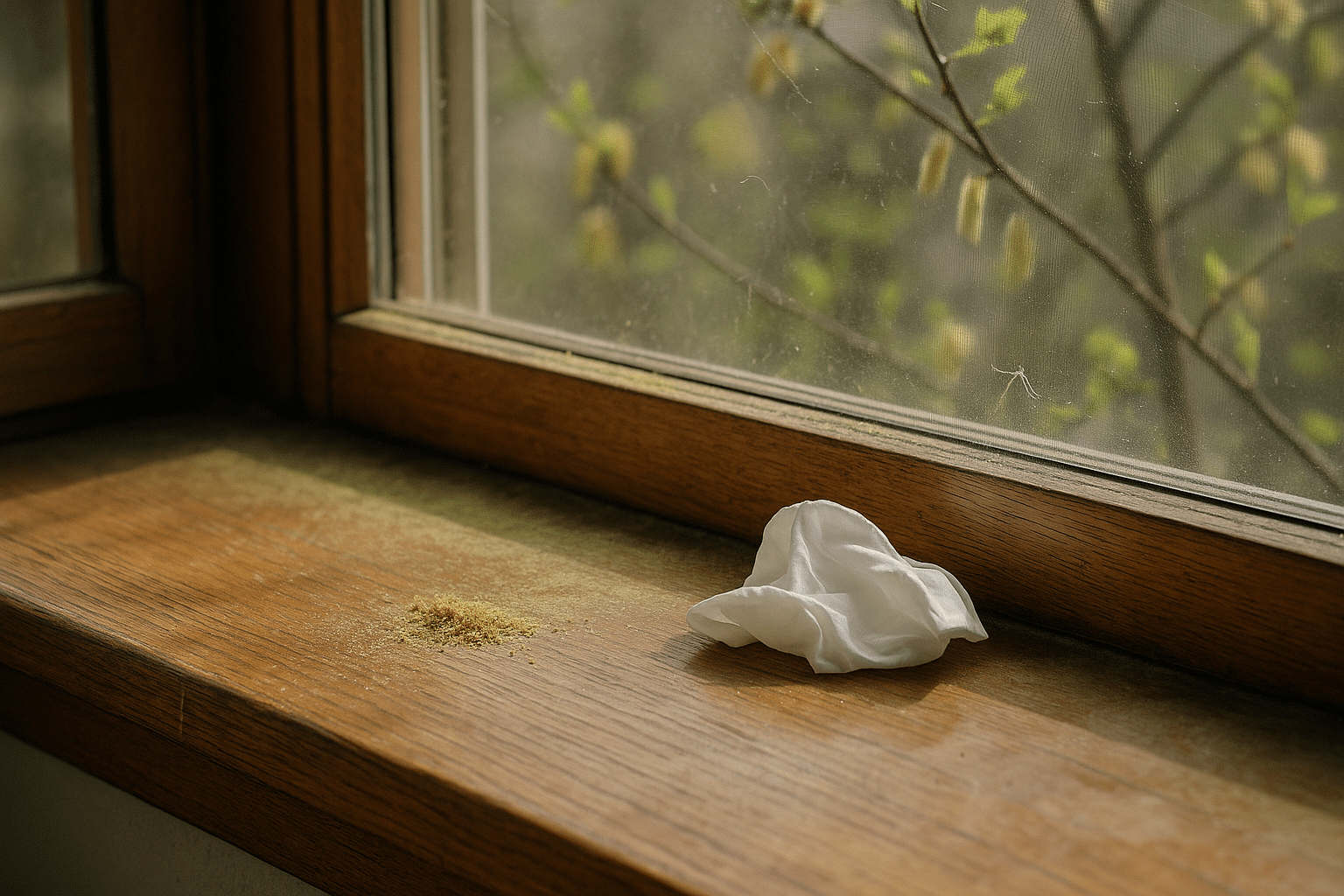
Many people see meaningful improvement by combining environment tweaks with targeted therapies. Saline irrigation—using isotonic or slightly hypertonic rinses—helps clear allergens, thin secretions, and support ciliary function. Consistency is more important than intensity: a gentle rinse once or twice daily during flare periods can be effective. Keep devices clean and use sterile or distilled water per safety guidance. Humidification can relieve dryness in winter; aim for moderate indoor humidity to reduce congestion without encouraging mold.
Allergen and irritant management can lighten the load:
– For pollens: check local counts; keep windows closed on high days; shower after outdoor time; dry laundry indoors during peak seasons
– For dust mites: use allergen-proof encasements for pillows and mattresses; wash bedding in hot water weekly; reduce bedroom clutter and vacuum with a HEPA-equipped machine
– For pets: create pet-free zones (especially the bedroom); use washable throws; bathe pets as advised for dander reduction
– For molds: fix leaks, improve ventilation, and clean visible growth with appropriate methods
Medication choices depend on symptoms and frequency. Intranasal corticosteroids are widely recommended as a cornerstone for persistent allergic rhinitis, helping relieve congestion, sneezing, itching, and runny nose by calming inflammation; full benefit may build over several days. Intranasal antihistamines act quickly and can be useful for sneezing and rhinorrhea, with some benefit for congestion. Oral antihistamines are convenient for intermittent symptoms, especially itching and sneezing, though they may be less helpful for congestion. An intranasal anticholinergic option targets watery drip and is particularly useful for nonallergic rhinorrhea. Short-term use of topical nasal decongestants can shrink swelling rapidly, but using them for more than a few days risks rebound congestion; if considered, it should be brief and carefully timed. Some individuals gain additional benefit from leukotriene-receptor blockers, especially with coexisting asthma or certain sensitivities; responses vary.
For confirmed allergic drivers, allergen immunotherapy (administered under medical supervision) may lessen sensitivity over time and reduce medication needs. This approach requires commitment and careful selection of target allergens but can offer durable symptom reduction for eligible patients. Non-drug measures complement everything: regular exercise, good sleep routines, hydration, and smoke-free environments support nasal health. The key is personalization—matching therapies to your symptom profile, triggers, and preferences—while giving each approach enough time to work before changing course.
Living Well with Rhinitis: Prevention, Routines, and Special Situations
Daily rhythms can either amplify rhinitis or smooth it out. Building a simple routine makes symptoms more predictable. For instance, a morning saline rinse during high-pollen weeks, followed by your chosen intranasal therapy, sets the tone for the day. Plan outdoor exercise when counts are lower or after rainfall, and keep a flexible toolkit: sunglasses to shield eyes from windborne particles, a light scarf for cold-air triggers, and a small bottle of saline spray for dry environments. If fragrances or cleaning sprays set you off, designate fragrance-free zones at home and ventilate well when using household products.
Sleep and workspace matter. Elevating the head of the bed slightly, using encasements, laundering bedding regularly, and running a clean, appropriately sized air purifier in the bedroom can reduce nighttime congestion. At work, position desks away from drafty vents, and discuss sensible scent policies if perfumes cause issues. For travel, sealable bags keep clothing separate from pet dander exposures; consider a portable HEPA unit for longer stays, and check hotel rooms for visible dampness before settling in.
Special populations benefit from tailored choices. Children may show irritability or mouth breathing more than they verbalize symptoms; routines and gentle rinses can help, and treatments should be age-appropriate. During pregnancy, non-drug measures are often emphasized first; some medications have established safety profiles, but decisions should be individualized with clinician input. Older adults might prioritize therapies with minimal drying or sedating effects. Athletes can experiment with warm-up breathing through the nose or a light face covering in cold weather to temper reflex congestion. Food-triggered “gustatory” rhinitis responds to simple strategies like moderating spice intensity or preemptive, targeted nasal therapy before meals when appropriate.
Finally, consider a practical action plan:
– List your top three triggers and one step to lessen each
– Choose a consistent daily habit (e.g., saline rinse) and track how you feel for two weeks
– Set a calendar reminder for filter changes and bedding care
– Keep a low-key symptom journal to spot patterns and wins
Progress with rhinitis often comes from steady, small moves rather than dramatic changes. With informed choices and a routine that fits your life, you can reduce the noise of symptoms and get back to the activities that matter.
Conclusion
Rhinitis is common, but it doesn’t have to run the show. By understanding your triggers, choosing treatments that match your symptoms, and shaping a few reliable habits, you can dial down congestion, sneezing, and drip. If you’re unsure which path to take, a brief conversation with a healthcare professional can clarify options and streamline your plan. Start small, stay consistent, and measure what works—breathing easier is a realistic, stepwise goal.